Brain Health
“Obsessive Compulsive Disorder (OCD) Is Ruining Your Life? Learn How To Cope With”

Obsessive-Compulsive Disorder (OCD) is a silent but debilitating condition that can invade every aspect of a person’s life. It’s an invisible monster that lurks in the corners of the mind, wreaking havoc on one’s days and nights. However, there is hope, and understanding how to cope with OCD can be the first step towards reclaiming a sense of control and normalcy.
Understanding OCD: The Intrusive Thoughts and Compulsions
OCD is characterized by two main components: obsessions and compulsions. Obsessions are intrusive, distressing, and persistent thoughts, images, or urges that cause significant anxiety. These obsessions often center around themes like cleanliness, safety, harm, or symmetry. They can be profoundly disturbing, making it difficult for individuals to focus on anything else.
Compulsions, on the other hand, are repetitive behaviors or mental acts that individuals with OCD feel compelled to perform in response to their obsessions. These actions are meant to reduce the anxiety and distress caused by the obsessions. For example, someone with a fear of germs might engage in excessive handwashing as a compulsion.
The Vicious Cycle: How OCD Takes Control
The vicious cycle of OCD begins with the onset of obsessions. These intrusive thoughts create intense anxiety, and individuals often believe that engaging in compulsions is the only way to alleviate that anxiety. Initially, compulsions may provide a temporary sense of relief, but this relief is short-lived. Over time, compulsions become a way of coping with the anxiety, and the cycle perpetuates itself.
As the cycle continues, OCD can consume a significant amount of time and energy. People with OCD often spend hours each day performing compulsions or engaging in mental rituals. This can disrupt daily routines, interfere with work or school, and strain relationships.
Coping with Obsessive Compulsive Disorder: A Step Towards Recovery
While OCD can be an overwhelming and persistent condition, there are effective ways to cope with it and regain control of your life.
1. Seek Professional Help: The first and most crucial step is to seek professional help. Cognitive-behavioral therapy (CBT) and medication, such as selective serotonin reuptake inhibitors (SSRIs), have been shown to be effective in treating OCD. A mental health professional can work with you to develop a treatment plan tailored to your specific needs.
2. Educate Yourself: Knowledge is power. Learn as much as you can about OCD, its symptoms, and treatment options. Understanding the condition can help demystify it and reduce the fear associated with obsessions.
3. Practice Mindfulness: Mindfulness techniques, such as meditation and deep breathing, can help you stay present and reduce anxiety. Mindfulness can also be used to resist the urge to engage in compulsions.
4. Exposure and Response Prevention (ERP): ERP is a specific form of CBT that involves deliberately exposing yourself to situations that trigger obsessions and then resisting the urge to perform compulsions. Over time, this can help reduce the anxiety associated with obsessions.
5. Build a Support System: Share your struggle with trusted friends and family members. Having a support system can provide emotional assistance and understanding during difficult times.
6. Keep a Journal: Record your obsessions, compulsions, and the situations that trigger them. This can help you and your therapist identify patterns and develop strategies to cope with them.
7. Set Realistic Goals: Recovery from OCD is a gradual process, and setbacks are common. Set realistic goals for yourself and celebrate your progress, no matter how small.
Conclusion
Obsessive Compulsive Disorder is a formidable opponent, but it is not invincible. With the right treatment, support, and coping strategies, individuals with OCD can regain control over their lives. Remember that seeking professional help is essential, as OCD is a complex condition that often requires expert guidance.
While it may feel like OCD is destroying your days and nights, there is hope, and recovery is possible. Each step you take towards coping with OCD brings you closer to a brighter and more fulfilling future, free from the chains of obsession and compulsion.
Brain Health
Bipolar Disorder: Symptoms, Subtypes, Causes, and Treatment Options

Bipolar disorder, formerly known as manic-depressive illness, is a complex and challenging mental health condition that affects millions of people worldwide. Characterized by dramatic mood swings, this disorder can disrupt a person’s life, relationships, and overall well-being.
In this article, we will explore the symptoms, subtypes, underlying causes, and various treatment options available for individuals living with bipolar disorder.
Understanding Bipolar Disorder
Bipolar disorder is characterized by distinct mood episodes that range from extreme highs, known as manic episodes, to profound lows, called depressive episodes.
These mood swings can vary in duration and intensity, and they significantly impact a person’s daily life and functioning.
Symptoms of Bipolar Disorder

Bipolar Disorder Symptoms: Manic Phase vs Depressed Phase
I- Depressive Episodes
During depressive episodes, individuals with bipolar disorder often experience the following symptoms:
1. Overwhelming Sadness: A pervasive sense of sadness, hopelessness, and despair that lasts for weeks or even months.
2. Fatigue: A persistent feeling of exhaustion, even after a full night’s sleep.
3. Loss of Interest: Diminished interest or pleasure in activities once enjoyed.
4. Sleep Disturbances: Insomnia or excessive sleep can disrupt sleep patterns.
5. Changes in Appetite: Significant changes in appetite leading to weight gain or loss.
6. Difficulty Concentrating: Trouble focusing, making decisions, or remembering things.
7. Feelings of Guilt: Excessive guilt, self-blame, and self-criticism.
8. Thoughts of Death: Recurrent thoughts of death, suicide, or self-harm.
II- Manic Episodes
Manic episodes are characterized by a distinct set of symptoms, including:
1. Elevated Mood: An unusually elevated, euphoric, or irritable mood.
2. Increased Energy: A surge in energy levels, leading to heightened activity.
3. Impulsivity: Engaging in reckless behavior, such as excessive spending, risky sexual encounters, or substance abuse.
4. Decreased Need for Sleep: Feeling rested with very little sleep.
5. Racing Thoughts: Thoughts that race, making it difficult to concentrate.
6. Grandiose Ideas: Believing in one’s exceptional abilities or importance.
7. Irritability: Heightened irritability and agitation.
Subtypes of Bipolar Disorder

Bipolar disorder is not a one-size-fits-all condition; it exists in different subtypes, each with its unique characteristics:
1. Bipolar I Disorder: This subtype involves manic episodes lasting at least seven days or severe enough to require hospitalization. Depressive episodes may also occur.
2. Bipolar II Disorder: Individuals with Bipolar II experience recurrent depressive episodes and hypomanic episodes, which are less severe than full-blown mania but still disruptive.
3. Cyclothymic Disorder: This milder form of bipolar disorder involves numerous periods of hypomanic and depressive symptoms over at least two years but doesn’t meet the criteria for manic or major depressive episodes.
4. Mixed Features: Some individuals experience both manic and depressive symptoms simultaneously, leading to a mixed episode.
Causes of Bipolar Disorder
While the exact cause of bipolar disorder remains uncertain, several factors are believed to contribute to its development:
- Genetics: A family history of bipolar disorder increases the risk, suggesting a genetic predisposition.
- Neurochemical Imbalance: Disruptions in brain neurotransmitters like dopamine and serotonin play a significant role in mood regulation.
- Stressful Life Events: Traumatic experiences, major life changes, or chronic stress can trigger episodes in individuals genetically predisposed to bipolar disorder.
- Brain Structure and Function: Research indicates that abnormalities in certain brain regions, including the prefrontal cortex and amygdala, are associated with bipolar disorder.
Treatment Options:
The management of bipolar disorder typically involves a multifaceted approach combining medication, psychotherapy, lifestyle changes, and support from healthcare professionals and loved ones.
- Medication: Mood stabilizers like lithium, anticonvulsants (e.g., valproate), and atypical antipsychotics (e.g., aripiprazole) are commonly prescribed to manage symptoms and prevent mood swings.Antidepressants are used cautiously in combination with mood stabilizers to address depressive episodes.
- Psychotherapy: Cognitive-behavioral therapy (CBT), psychoeducation, and interpersonal and social rhythm therapy (IPSRT) can help individuals better understand their condition, develop coping strategies, and maintain stable daily routines.
- Electroconvulsive Therapy (ECT): In severe cases or when other treatments are ineffective, ECT may be considered, particularly for individuals in a depressive or mixed state.
- Lifestyle Management: Maintaining a regular sleep schedule, managing stress, avoiding alcohol and substance abuse, and adhering to a healthy diet can help reduce the frequency and severity of mood swings.
- Support Network: Building a strong support system with family and friends is essential for individuals with bipolar disorder. Support groups and counseling can provide valuable assistance.
- Self-Monitoring: Keeping a mood diary to track mood swings, sleep patterns, and triggers can be helpful in managing the condition.
- Hospitalization: In severe cases where individuals pose a risk to themselves or others, hospitalization may be necessary to stabilize their condition.
Conclusion
Bipolar disorder is a challenging mental health condition that requires careful management and support.
By understanding its symptoms, recognizing its subtypes, exploring potential causes, and considering various treatment options, individuals living with bipolar disorder and their loved ones can navigate this complex condition more effectively.
Seeking professional help and maintaining a robust support system are essential steps towards achieving stability and improved quality of life for those affected by bipolar disorder.
Brain Health
Innovations in Schizophrenia Treatment in All 5 Ways: Advances in Medication and Therapy

Schizophrenia is a complex and debilitating mental disorder that affects millions of people worldwide. Historically, treatment options for schizophrenia have been limited and often carried significant side effects.
However, recent years have seen remarkable advancements in both medication and therapy, offering new hope and improved outcomes for individuals living with this condition. In this article, we will explore some of the most promising innovations in schizophrenia treatment.
1. Antipsychotic Medications

Antipsychotic medications have long been the cornerstone of schizophrenia treatment. However, recent innovations in this field have focused on improving efficacy and reducing side effects. One notable advancement is the development of second-generation antipsychotics, also known as atypical antipsychotics.
These medications, such as aripiprazole, olanzapine, and risperidone, have demonstrated a more favorable side effect profile compared to their older counterparts.
They target a broader range of symptoms, providing relief from hallucinations, delusions, and thought disorders. Additionally, long-acting injectable formulations have emerged, ensuring medication adherence and reducing relapse rates.
2. Personalized Medicine
Personalized medicine is revolutionizing the treatment of schizophrenia. By analyzing an individual’s genetics and response to medication, clinicians can tailor treatment plans to each patient’s unique needs.
Genetic testing helps identify specific genetic markers that may influence how a person responds to medication. This information allows for more precise medication selection and dosing, increasing the likelihood of treatment success while minimizing side effects.
3. Cognitive-Behavioral Therapy (CBT)

Cognitive-behavioral therapy has gained recognition as an effective adjunctive treatment for schizophrenia.
This evidence-based therapy helps individuals manage their symptoms, improve functioning, and enhance their quality of life. CBT focuses on challenging and reshaping distorted thought patterns, reducing distress associated with symptoms, and improving coping skills.
Innovations in CBT include the development of specialized programs tailored to address schizophrenia-related challenges.
Therapists utilize cognitive restructuring techniques to help individuals regain control over their thoughts, reduce the severity of hallucinations and delusions, and enhance their problem-solving abilities.
4. Social Skills Training
People with schizophrenia often struggle with social interactions, making it challenging to maintain relationships and hold down jobs. Social skills training programs have emerged as a valuable therapy option. These programs teach individuals with schizophrenia essential social skills, such as effective communication, problem-solving, and conflict resolution.
Innovations in social skills training incorporate technology, including virtual reality simulations, to create realistic social scenarios for practice. These immersive experiences provide a safe and controlled environment for individuals to develop and refine their social skills.
5. Early Intervention
Early intervention is critical in managing schizophrenia effectively. Advances in early detection and intervention have improved outcomes for individuals at risk or in the early stages of the illness. Comprehensive assessment tools and the recognition of early warning signs enable clinicians to intervene promptly.
Treatment during the prodromal or early stages of schizophrenia often involves a combination of medication and psychotherapy, with a focus on preventing the progression of symptoms and improving functioning. These early interventions can significantly reduce the long-term impact of the disorder.
Outcome:
The landscape of schizophrenia treatment has evolved significantly in recent years, offering hope and improved prospects for those affected by this complex mental illness.
Innovations in medication, personalized medicine, psychotherapies like CBT and social skills training, and a heightened emphasis on early intervention have collectively transformed the way we approach and manage schizophrenia.
These advances represent a shift toward a more holistic and patient-centered approach to treatment, where the unique needs of each individual are carefully considered.
While challenges remain in the field of schizophrenia treatment, these innovations provide a ray of hope for those living with the condition, promising better outcomes and an improved quality of life.
With ongoing research and continued investment in mental health care, we can look forward to even more promising developments in the future.
Brain Health
What are Benzodiazepines Uses? What are Their 3 Different Types and Thier Side Effects? A Detailed Discussion:

Benzodiazepines Uses is so common thing now a days. Benzodiazepines are a class of psychoactive drugs primarily used to treat anxiety, insomnia, and certain medical conditions.
They work by enhancing the activity of a neurotransmitter called gamma-aminobutyric acid (GABA), which helps calm the central nervous system. Here are some key points about benzodiazepines:
Types:
1. Short-acting benzodiazepines: These have a rapid onset of action and a shorter duration of effect. Examples include alprazolam (Xanax) and lorazepam (Ativan).
2. Intermediate-acting benzodiazepines: These have a moderate onset and duration of action. Examples include diazepam (Valium) and clonazepam (Klonopin).
3. Long-acting benzodiazepines: These have a slower onset and a longer duration of action. Examples include diazepam (Valium) and chlordiazepoxide (Librium).
When They Should Be Used:
Benzodiazepines should be used under the guidance of a healthcare professional and only for specific medical conditions such as:

Benzodiazepines Uses
– Anxiety disorders
– Panic disorder
– Insomnia (short-term use)
– Seizure disorders
– Alcohol withdrawal symptoms
– Muscle spasms
It’s important to note that they are typically prescribed for short-term use due to the risk of tolerance, dependence, and withdrawal symptoms.
Side Effects:
Common side effects of benzodiazepines may include:

Side Effects of Benzodiazepines
– Drowsiness
– Dizziness
– Confusion
– Memory problems
– Muscle weakness
– Impaired coordination
– Reduced alertness
Long-term or misuse of benzodiazepines can lead to dependence and withdrawal symptoms when trying to stop using them.
Additionally, they can interact with alcohol and other medications, leading to potentially dangerous consequences.
Benzodiazepines Withdrawal Symptoms:
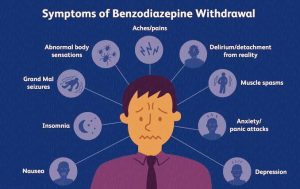
Withdrawal Symptoms
- Anxiety and panic attacks
- Insomnia and disrupted sleep patterns
- Irritability and mood swings
- Muscle tension and stiffness
- Nausea and vomiting
- Sweating and chills
- Tremors and shakiness
- Hallucinations or seizures in severe cases
- Increased heart rate and blood pressure
- Difficulty concentrating and memory problems
- Sensory hypersensitivity, such as heightened sensitivity to light and sound.
Benzodiazepines should be used cautiously, and it’s important to follow your healthcare provider’s instructions carefully to minimize the risks associated with their use. If you have concerns or experience side effects, consult your healthcare provider.
-

 Brain Health7 months ago
Brain Health7 months agoWhat are Benzodiazepines Uses? What are Their 3 Different Types and Thier Side Effects? A Detailed Discussion:
-

 Brain Health7 months ago
Brain Health7 months agoBipolar Disorder: Symptoms, Subtypes, Causes, and Treatment Options
-

 Brain Health7 months ago
Brain Health7 months agoInnovations in Schizophrenia Treatment in All 5 Ways: Advances in Medication and Therapy
-

 Women's Health7 months ago
Women's Health7 months agoUnderstanding Breast Cancer: Symptoms, Causes, and Treatments
-

 Men's Health7 months ago
Men's Health7 months agoLoss of Libido: Symptoms, Causes, and Management Techniques
-

 Women's Health5 months ago
Women's Health5 months agoPCOS Awareness: Shedding Light on a Common Women’s Health Issue
-

 Men's Health7 months ago
Men's Health7 months ago“Understanding Erectile Dysfunction: Causes, Treatment Options, and Management”
-

 Men's Health6 months ago
Men's Health6 months ago7 Foods that Enhance Your Testosterone Levels

